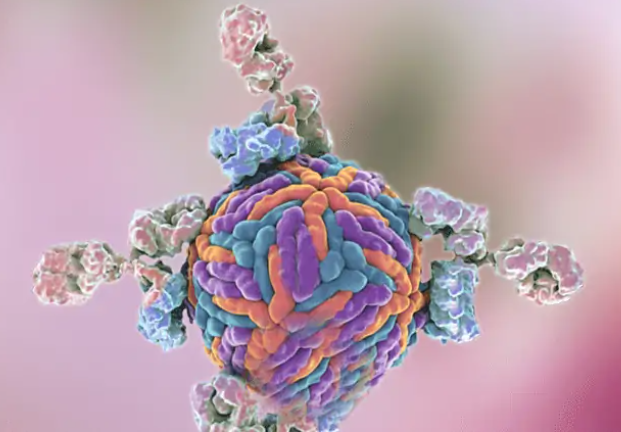
Immunotherapy stands out as the most promising systemic approach to cancer treatment compared to conventional methods. Monoclonal antibodies, known for their ability to precisely target molecules, have emerged as a vital and effective modality in cancer therapy. However, the intricacies of tumor development often limit the effectiveness of monoclonal antibodies targeting a single point. The introduction of bispecific antibodies (bsAbs), capable of targeting multiple sites simultaneously, has transformed the landscape of tumor immunotherapy.
What is a bispecific antibody? Over the last few decades, there has been a notable shift from developing and modifying basic antibodies (Abs) to more intricate Ab derivatives, with a special focus on bsAbs of varied shapes and sizes. BsAb technology holds tremendous promise in clinical applications, garnering researchers’ attention and evolving into diverse forms, establishing a robust foundation for cancer immunotherapy centered around bsAbs. Presently, a multitude of preclinical and clinical trials are underway, marking the era of bispecific antibodies in tumor immunotherapy. As of December 2021, the United States Food and Drug Administration (FDA) has granted approval for three types of bsAbs for clinical cancer treatment.
Due to their capability to simultaneously target two epitopes on tumor cells or within the tumor microenvironment (TME), bsAbs have become a pivotal and promising element of the next generation of therapeutic antibodies. The majority of bsAbs in current development are crafted as T-cell engagers, forging close connections between immune cells, particularly cytotoxic T cells, and tumor cells to create an artificial immune contact. This ultimately leads to selective attacks and lysis of targeted tumor cells.
Bispecific T-cell engagers, as a groundbreaking cancer immunotherapy strategy, have exhibited encouraging results in clinical trials, particularly in hematologic malignancies. To date, only one bispecific T-cell engager, blinatumomab, has received approval from the FDA and the European Medicines Agency for treating relapsed or refractory B-cell precursor acute lymphoblastic leukemia (B-ALL) and minimal residual disease (MRD)-positive B-ALL. Additionally, numerous other bispecific T-cell engagers are undergoing clinical trials, targeting various tumor types, including hematologic malignancies and solid tumors.
Classified by their functional mechanisms, bsAbs, besides cell-cell engagers, can be further divided into those binding two epitopes on the same antigen, dual-functional modulators, and bsAbs in cell therapy. One innovative form includes those with an antigen-binding Fc fragment (Fcab), incorporating a homodimeric Fc region with antigen-binding sites. This distinctive combination enables Fcabs to simultaneously leverage the functions mediated by the Fc domain and antigen-binding capabilities. Significantly, Fcabs are one-third smaller than full-length antibodies, facilitating superior tissue penetration, particularly advantageous in treating solid tumors. Moreover, Fcabs serve as a robust foundation for creating antibody-drug conjugates (ADCs), ensuring precise drug delivery by linking cytotoxic drugs specifically to Fcab.
While most bsAbs in clinical trials presently target hematologic malignancies, exploring bsAbs targeting solid tumors is essential due to their inevitable adverse effects on normal tissues. Factors like immune-tolerant cancer stroma, angiogenic disorders, and insufficient penetration of bsAb drugs contribute to the complexity of this exploration. As a result, there is enthusiastic interest in ongoing research on bsAbs in solid tumors. In conclusion, the outcomes of bsAb research underscore the promising prospects of these molecules in innovative drug design and subsequent clinical applications in cancer treatment.